optimys
MATHYS
optimys
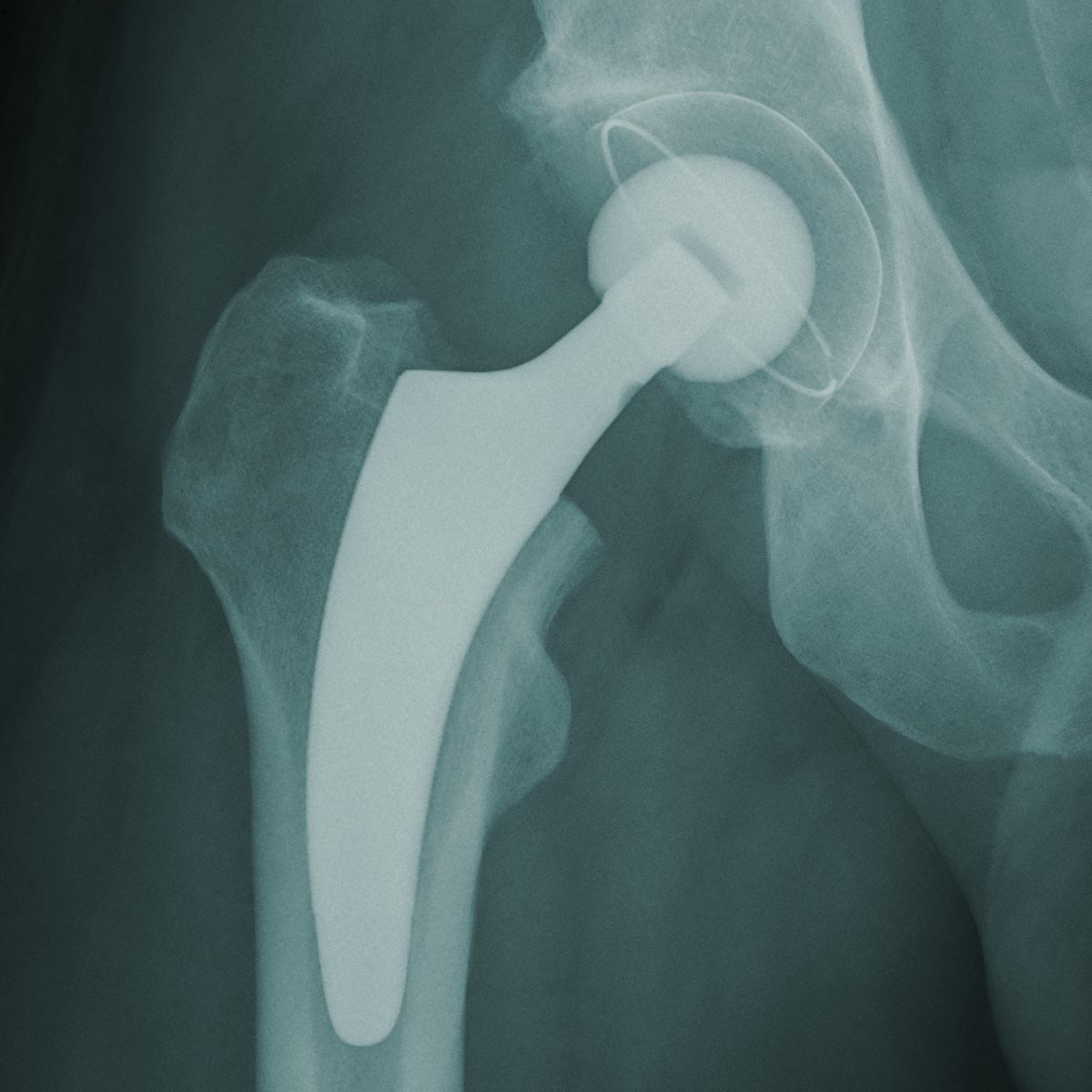
Stem guided by the calcar femorale
The optimys stem was developed to allow reconstruction of the individual patient’s anatomy. The key anatomical landmark for implanting the stem is the medial curvature of the femur, allowing the objective of restoration of the centre of rotation and offset to be achieved, regardless of the initial varus or valgus position of the femoral neck.1, 2
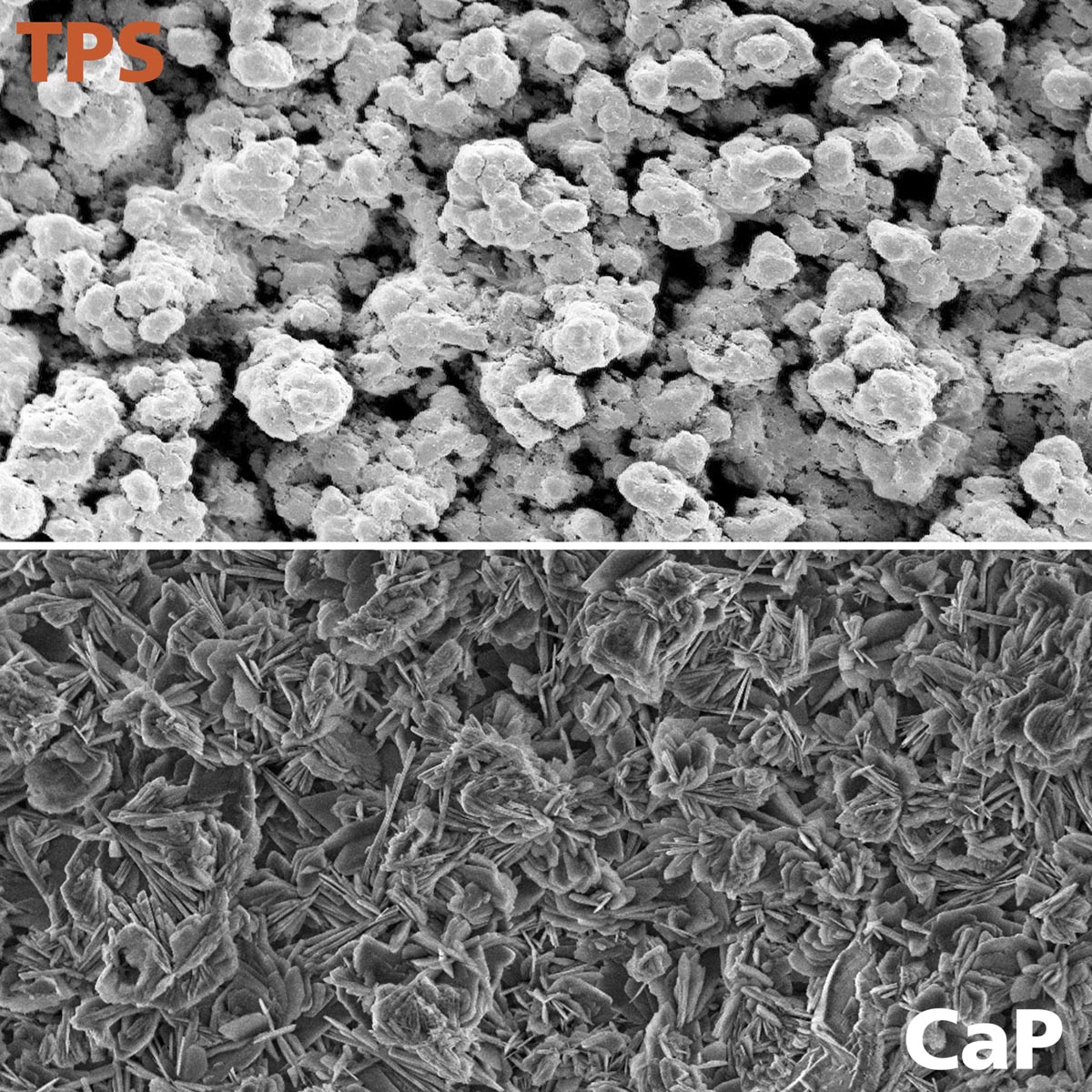
The philosophy of the optimys stem focuses on the medial curvature of the femur (calcar femorale). The result is the stem can be adapted to the patient’s individual anatomical conditions with the goal of reconstructing the patient’s offset.1, 2 The distinctive triple taper design allows good primary stability to be achieved to minimise the risk of subsidence postoperatively.3, 4, 5 The titanium plasma spray with calcium phosphate coating promotes osseointegration of the stem.
With twelve sizes for the standard and lateral version, the system offers a comprehensive implant portfolio.
The optimys stem, in combination with a Mathys ceramic head and the RM Pressfit vitamys cup, is known as the bonepreservation system.
Update: The Enovis and Mathys product range is now exclusively available through LimaCorporate in the UK. Osteotec remains the distributor for Enovis and Mathys customers in Ireland (Republic of Ireland and Northern Ireland) and the Nordics (Norway, Sweden, Denmark, and Finland).
Enquire
For further information, questions regarding this product, or to discuss alternative solutions, please get in touch with your local Sales Specialist or our Head Office using the form or the contact details at the bottom of the page.
Stay in touch
NEWSLETTER
Sign up to receive email updates on new product announcements, insights on surgical techniques from surgeons, specialists, and sales representatives and industry trends, such as changes in regulations and new research findings.